SARS-CoV-2 infections may induce neuroinflammation ucdavis CellPressNews SARSCoV2 COVID19 Neuroinflammation Infection
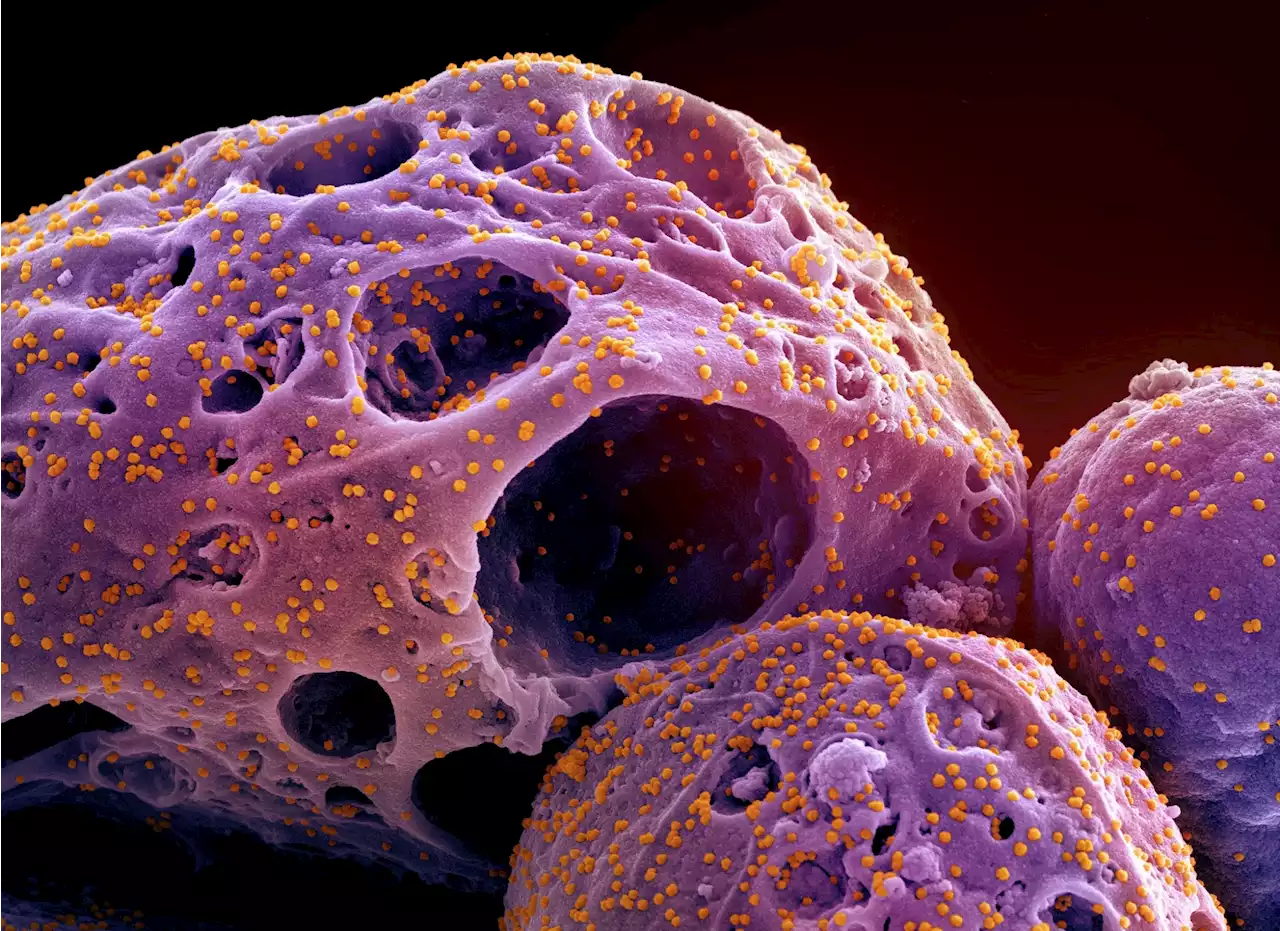
By Bhavana KunkalikarNov 3 2022Reviewed by Aimee Molineux In a recent study published in Cell Reports, researchers assessed the impact of severe acute respiratory syndrome coronavirus 2 on neuroinflammation.
This study used 14 colony-bred male and female rhesus macaques of Indian origin. The two main age groups for the animals were young adults aged between four and 12 years and older subjects aged 18 to 24. Three subgroups of young adults and older subjects were identified: infected non-type-2 diabetics, non-infected type-2 diabetics, and non-infected non-diabetics.
Results Cell-type analysis showed that in the young as well as old animals, the SARS-CoV-2 nucleocapsid immunosignal colocalized with astrocytes , microglia , and neurons . Neurons had the highest level of intracellular N protein irrespective of age. At the same time, elderly animals revealed higher quantities than young animals across all three cell types, according to volume quantification of intracellular N protein by cell type.
When young, infected animals were compared to their corresponding age-matched, non-infected controls, there was a rise in the number of astrocytes. Notably, GFAP populations significantly increased in both young and old infected mice, suggesting either astrocyte growth or translocation to the piriform cortex.
Australia Latest News, Australia Headlines
Similar News:You can also read news stories similar to this one that we have collected from other news sources.
 Frontiers | SARS-CoV-2 specific antibody trajectories in mothers and infants over two months following maternal infectionInfants exposed to caregivers infected with SARS-CoV-2 may have heightened infection risks relative to older children due to their more intensive care and feeding needs, and may experience more severe infection due to their less developed immune systems. However, there has been limited research on COVID-19 outcomes in exposed infants beyond the neonatal period. Between June 2020 – March 2021, we conducted interviews and collected capillary dried blood from SARS-CoV-2 infected mothers and their infants (aged 1-36 months) for up to two months following maternal infection onset (COVID+ group, 87% breastfeeding, n dyads=46 dyads). Comparative data were also collected from breastfeeding mothers with no known SARS-CoV-2 infection or exposures (breastfeeding control group, n dyads=26), and mothers who tested SARS-CoV-2 negative after experiencing symptoms or close contact exposure (COVID- group, n dyads=11, 73% breastfeeding). Dried blood samples were assayed for anti-SARS-CoV-2 S-RBD IgG and IgA positivity and anti-SARS-CoV-2 S1 + S2 IgG concentrations. Within the COVID+ group, the mean probability of seropositivity among infant samples was significantly lower than that of corresponding maternal samples (IgG 0.54 vs. 0.87; IgA 0.33 vs. 0.85), with likelihood of infant infection positively associated with the number of maternal symptoms and other household infections reported. COVID+ mothers reported a lower incidence of COVID-19 symptoms among their infants as compared to themselves and other household adults, and infants had similar PCR positivity rates as other household children. No samples returned by COVID- mothers or their infants tested antibody positive. Among the breastfeeding control group, 44% of mothers but none of their infants tested antibody positive in at least one sample. Results support previous research demonstrating minimal risks to infants following maternal COVID-19 infection, including for breastfeeding infants.
Frontiers | SARS-CoV-2 specific antibody trajectories in mothers and infants over two months following maternal infectionInfants exposed to caregivers infected with SARS-CoV-2 may have heightened infection risks relative to older children due to their more intensive care and feeding needs, and may experience more severe infection due to their less developed immune systems. However, there has been limited research on COVID-19 outcomes in exposed infants beyond the neonatal period. Between June 2020 – March 2021, we conducted interviews and collected capillary dried blood from SARS-CoV-2 infected mothers and their infants (aged 1-36 months) for up to two months following maternal infection onset (COVID+ group, 87% breastfeeding, n dyads=46 dyads). Comparative data were also collected from breastfeeding mothers with no known SARS-CoV-2 infection or exposures (breastfeeding control group, n dyads=26), and mothers who tested SARS-CoV-2 negative after experiencing symptoms or close contact exposure (COVID- group, n dyads=11, 73% breastfeeding). Dried blood samples were assayed for anti-SARS-CoV-2 S-RBD IgG and IgA positivity and anti-SARS-CoV-2 S1 + S2 IgG concentrations. Within the COVID+ group, the mean probability of seropositivity among infant samples was significantly lower than that of corresponding maternal samples (IgG 0.54 vs. 0.87; IgA 0.33 vs. 0.85), with likelihood of infant infection positively associated with the number of maternal symptoms and other household infections reported. COVID+ mothers reported a lower incidence of COVID-19 symptoms among their infants as compared to themselves and other household adults, and infants had similar PCR positivity rates as other household children. No samples returned by COVID- mothers or their infants tested antibody positive. Among the breastfeeding control group, 44% of mothers but none of their infants tested antibody positive in at least one sample. Results support previous research demonstrating minimal risks to infants following maternal COVID-19 infection, including for breastfeeding infants.
Read more »
 Exploring trends in SARS-CoV-2 RNA concentrations in wastewaterExploring trends in SARS-CoV-2 RNA concentrations in wastewater medrxivpreprint Stanford EmoryUniversity SARSCoV2 COVID19 RNA Wastewater
Exploring trends in SARS-CoV-2 RNA concentrations in wastewaterExploring trends in SARS-CoV-2 RNA concentrations in wastewater medrxivpreprint Stanford EmoryUniversity SARSCoV2 COVID19 RNA Wastewater
Read more »
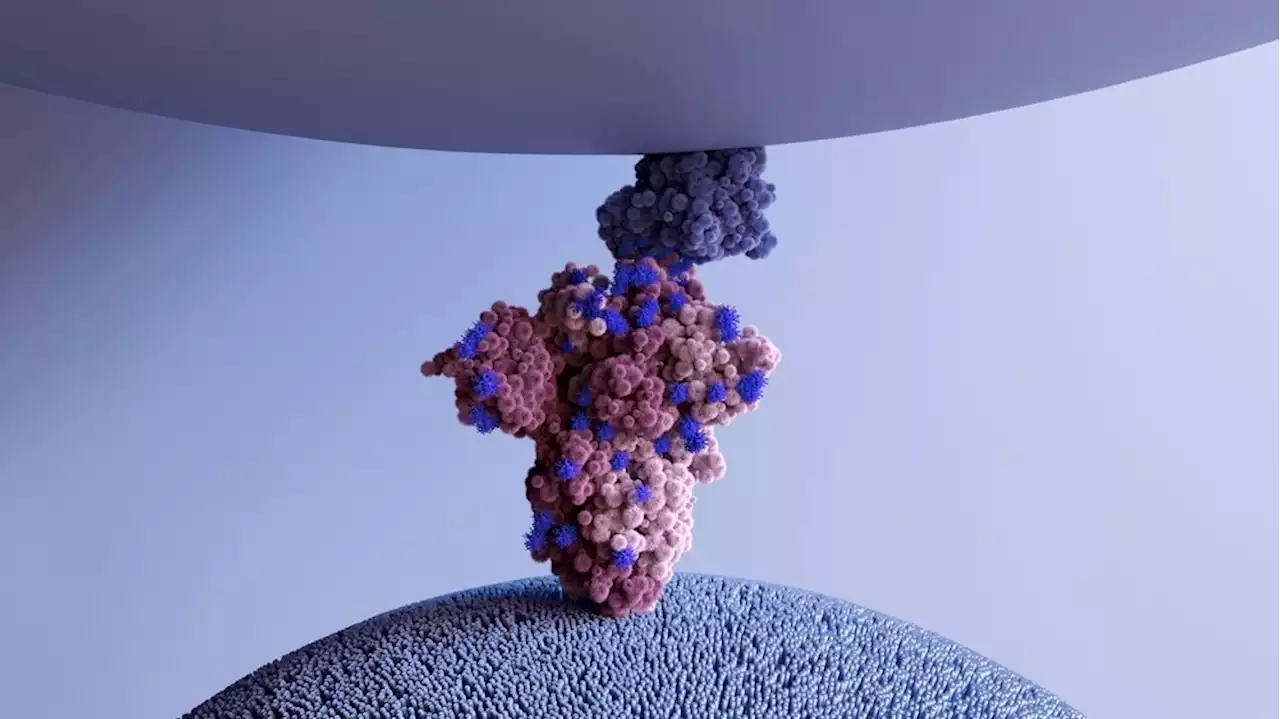 Vimentin is an important co-receptor for SARS-CoV-2 infectionVimentin is an important co-receptor for SARS-CoV-2 infection Receptor SARSCoV2 Coronavirus Disease COVID ACE2 Vimentin iScience_CP IHU_Marseille univamu
Vimentin is an important co-receptor for SARS-CoV-2 infectionVimentin is an important co-receptor for SARS-CoV-2 infection Receptor SARSCoV2 Coronavirus Disease COVID ACE2 Vimentin iScience_CP IHU_Marseille univamu
Read more »
 Bivalent mRNA booster broadens humoral immunity against SARS-CoV-2 Omicron subvariantsResearchers at Emory University, Stanford University, and the National Institute of Allergy and Infectious Diseases evaluated whether bivalent coronavirus disease 2019 (COVID-19) boosters conferred protection against new Omicron subvariants.
Bivalent mRNA booster broadens humoral immunity against SARS-CoV-2 Omicron subvariantsResearchers at Emory University, Stanford University, and the National Institute of Allergy and Infectious Diseases evaluated whether bivalent coronavirus disease 2019 (COVID-19) boosters conferred protection against new Omicron subvariants.
Read more »
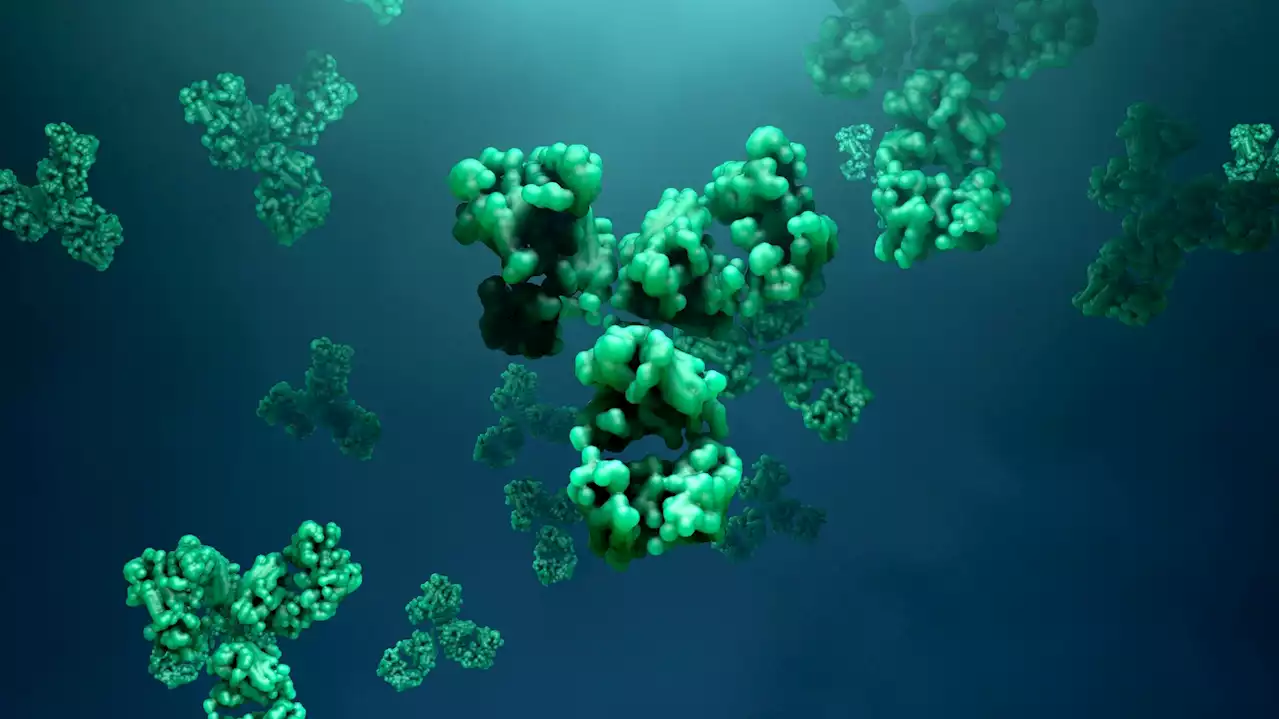 Scientists identify a broadly neutralizing antibody against all dominant SARS-CoV-2 variantsScientists identify a broadly neutralizing antibody against all dominant SARS-CoV-2 variants Antibody SARSCoV2 Coronavirus Disease COVID biorxivpreprint WeillCornell UWMadison scrippsresearch UChicago IcahnMountSinai seattlechildren
Scientists identify a broadly neutralizing antibody against all dominant SARS-CoV-2 variantsScientists identify a broadly neutralizing antibody against all dominant SARS-CoV-2 variants Antibody SARSCoV2 Coronavirus Disease COVID biorxivpreprint WeillCornell UWMadison scrippsresearch UChicago IcahnMountSinai seattlechildren
Read more »
 How does imprinted SARS-CoV-2 humoral immunity drive convergent Omicron evolution?How does imprinted SARS-CoV-2 humoral immunity drive convergent Omicron evolution? evolution SARSCoV2 immunity COVID19 coronavirus covid Omicron
How does imprinted SARS-CoV-2 humoral immunity drive convergent Omicron evolution?How does imprinted SARS-CoV-2 humoral immunity drive convergent Omicron evolution? evolution SARSCoV2 immunity COVID19 coronavirus covid Omicron
Read more »
